A basic necessity of life, food nourishes our very existence. Lucy is now adjusting to her new feeding friend after a long-anticipated procedure, a PEG insertion. This 'lifeline' is a bittersweet compromise ...

Hi, Everyone!
I was in theatre recently, undergoing Gastrostomy surgery. For those who don't know, a Gastrostomy is a surgical procedure where a feeding tube is placed directly into the stomach. This would allow me to get the nutrition I need without having to rely on my oral intake alone, which is challenging for me due to my digestive disorders. I can still eat small amounts, but not enough to sustain myself. It's a common misconception that people with feeding tubes can't eat anything. But it all depends on each person’s individual situation. I can manage small portions of softer foods, but another person with a feeding tube might not be able to eat at all. For me, it helps me maintain my nutritional needs, since eating regular meals is difficult due to my GI & Oesophageal dysmotility. As I tried to prepare for the day ahead, I was consumed by a whirlwind of emotions- Including nervousness and relief. I knew this procedure was necessary and would make day-to-day life easier for me, but I was also very much aware of the fact that this would be a significant adjustment and could be challenging. For the last nineteen months, I'd been relying on nasogastric tubes for feeding and essential nutrition. I'd been through multiple NG tube replacements during this time, some of which have been truly unpleasant. But they've still been a helpful tool and have effectively provided me with the nutrition I needed. But they aren't meant for long-term use, as they can dislodge or cause irritation and discomfort. So, my medical team and I decided that transitioning to a Percutaneous Endoscopic Gastrostomy (PEG) tube would be a better long-term solution. It would be more secure, less visible, and hopefully easier to manage.
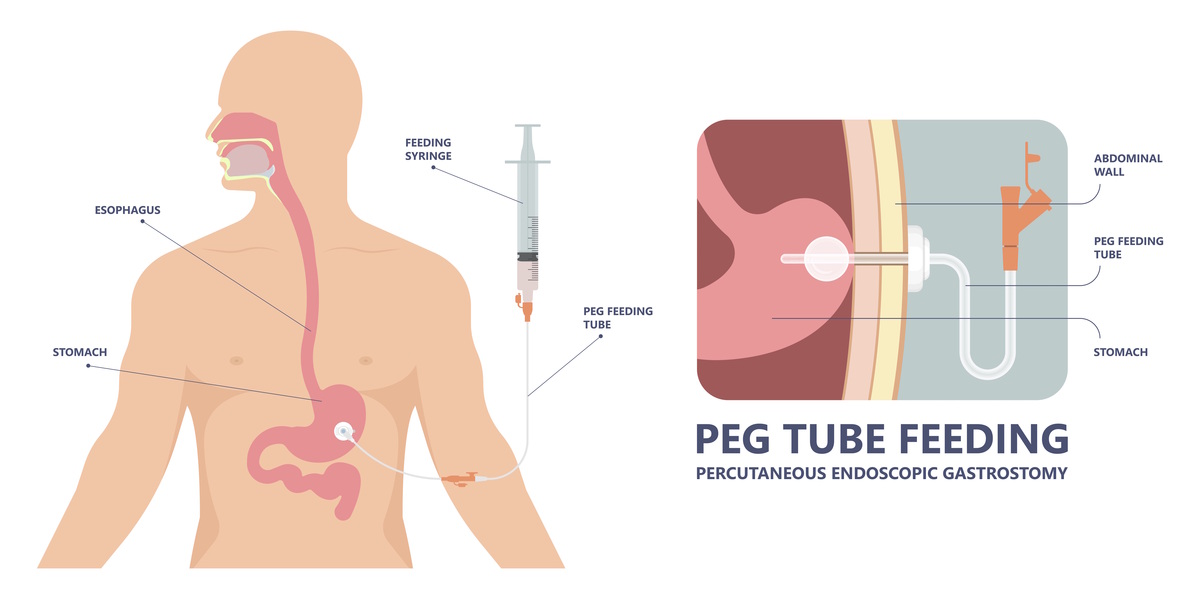
Switching to a PEG wasn't an easy decision to make. I weighed up the pros and cons with my medical team for a long time before I finally decided to agree. I'm used to NG tubes, but they require regular re-insertion because they aren't made to last. While they've served their purpose, I have been growing tired of constantly having them taped to my face. PEG tubes, on the other hand, can stay in place much longer without needing any adjustments. They also offer greater comfort and stability. Although I am nervous about the upcoming surgery, I am relieved that it is finally happening after several delays. Despite my anxiety, I am focusing on the positive impact this procedure will have on my quality of life. After being admitted to the hospital, I underwent some final observations before being taken to the operating room. My blood tests, blood pressure, and heart rate were all normal. Despite my fears about potential complications, I was ready to bid farewell to my latest NG tube after nineteen long months. The nurse removed it when I arrived at the theatre, and while I was glad to be rid of it, it was bittersweet knowing I would never have to endure another NG tube replacement.
The procedure itself was relatively straightforward and took about 30 minutes altogether. I don’t remember much of it, but after administering a sedative, the doctor inserted a small camera through my mouth to guide the placement of the feeding tube into my stomach. Once in place, they created a small incision in my abdomen to secure the tube. I didn’t feel anything, but because I was only under conscious sedation, I was somewhat aware during the procedure and recall watching the nurses cleaning blood off my stomach afterwards. I remember looking down at the small tube extending from my abdomen. It was strange at first, but knowing that this tube would help me maintain my nutritional requirements made it feel like a lifeline rather than an inconvenience. The nurses assured me that I would easily adjust to the changes, but in addition to feeling relieved, I also felt overwhelmed. I was unsure if I could handle the responsibility of caring for an important medical device. However, the surgery went well and despite experiencing some stomach discomfort, I was able to manage the pain. I was transported back to the ward after a brief stay in the recovery room. A few hours later, the nurses came round to guide me through the basics of post-op care. They explained how to care for the incision site and reassurred me that the soreness would gradually ease. They intended to discharge me the following morning, but my POTS symptoms started to flare up and my obs weren't great, so I ended up spending a few days on the ward. I got home eventually though, and I was glad that the surgery was behind me and I could now try to move forward with my new feeding friend.