Newly elevated to the status of ‘organ in its own right’ by the European Association for Cardio-Thoracic Surgery (EACTS), the aorta now sits on a par with the heart and brain. But what does this mean in clinical practice for something once viewed as “just a tube”? In the following piece we translate the EACTS’s new guidelines into the context of Marfan syndrome. We also discuss the Marfan aorta.
Background
The aorta is responsible for carrying oxygen-rich blood from the heart to the rest of the body. However, it has become increasingly evident that it also plays an instrumental role in regulating blood pressure and blood flow velocity. In 2022, the EACTS council commissioned the review and revision of the guidelines treating acute and chronic syndromes of the aorta. Until now, aortic diseases had usually been treated either in cardiac surgery or in vascular surgery, depending on their type and location.
The Aorta in Marfan Syndrome
Marfan syndrome is characterised by a lack of connective tissue elasticity and this can compromise the wall of the aorta, causing it to dilate, bulge and tear (dissect).
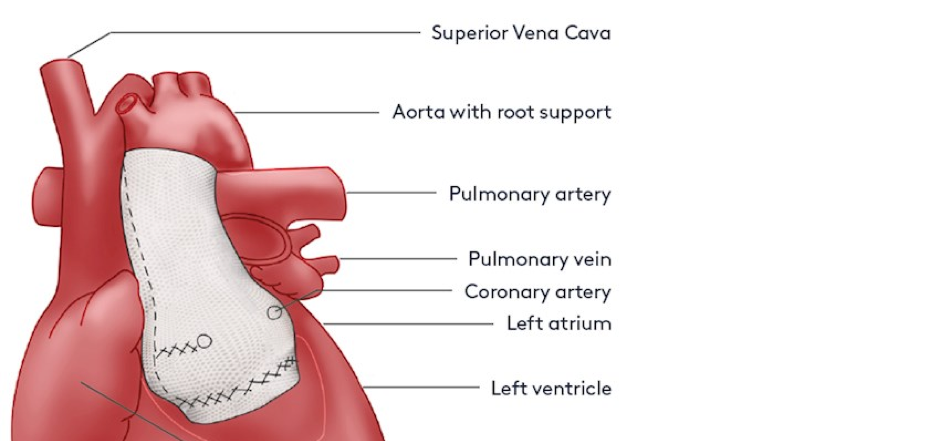
Our body’s largest artery, the aorta arises directly from the heart’s left ventricle and all blood pumped from the heart must first pass into this artery. After leaving the heart, the aorta branches into large vessels that carry oxygen-rich blood to the entire body. A valve, the aortic valve, lies between the left ventricle and the aorta and functions to keep blood, once pumped out to the aorta from leaking back to the heart.
The wall of the aorta consists of three parts:
1) A thin, inner layer (intima) is the ‘tube’ through which the blood passes. It contains smooth muscle tissue, connective tissue and endothelial cells. These special cells enable blood to transport oxygen and nutrients without getting absorbed until it reaches the right spot.
2) A thick, elastic middle layer (media). This layer is made of smooth muscle tissue, elastin and collagen (proteins). These substances enable the aorta to meet your body’s changing blood flow needs. When more blood is necessary, the aorta widens. If less blood is needed, it narrows.
3) An outer layer (adventitia). The outer layer anchors the aorta in place. It also connects to nearby nerves and tissue.
In Marfan syndrome, the middle layer, the media is weaker than normal. Year after year, as the aortic wall faces the constantly changing stress generated by the beating heart, the wall, particularly in the aortic root which is the first two or four inches above the aortic valve (sinuses of Valsalva) can gradually stretch. In this region, the diameter of the aorta, usually about one and a half inches (3.7cm) in an adult, widens (dilates). This dilated region is known as an aortic aneurysm. When the enlargement reaches 4.5cm, surgery is considered. If untreated, and the aortic root is left to widen, it may develop a tear – dissection - in the wall. This tear may proceed downward through the middle layer of the aorta through which blood rushes causing the inner layer to also tear which constitutes a dissection. This is the most serious complication someone with Marfan syndrome can suffer. It is a time-critical medical emergency that when diagnosed and treated quickly has a better than 80% survival rate.
The beginning portion of the aorta – the root - dilates to some degree in nearly everyone with Marfan syndrome. The echocardiogram is the simplest method for detecting and measuring the aorta in this region. This enlargement usually begins quite early in life and is detectable using echocardiography in most infants with the condition. It can be managed medically with beta-blockers and angiotensin receptor blockers if or until elective surgery is required.
New Guidelines in the Context of Marfan Syndrome
In recent years the aorta has been increasingly viewed by the medical profession as “more than just a tube”. Doctors began taking a holistic approach some time ago to diseases of the aorta (aortopathies), treating them in a multi-disciplinary context. This new attitude has steadily evolved, becoming cemented in the EACTS Guidelines which were published simultaneously with the aorta’s new classification as the ‘body’s 24th organ’. Leading the development of these new guidelines was Professor Martin Czerny from the University of Freiburg.
As Professor Czerny says: “The new guidelines clearly recommend bundling the treatment of the aorta in a separate speciality, in close coordination with other specialities. We have been practising this integrative approach at the Medical Center - University of Freiburg for a long time and I am delighted that our work is now also being recognised internationally,"
This is already starting to be practised in the United Kingdom with the creation of aortic teams within many hospitals . These new guidelines will support their development and help collaborative working and the creation of a streamlined approach to patients who need lifelong care and surveillance, like the Marfan community.
The health professionals needed to work together in a team providing care (the list is not exhaustive).
· Cardiothoracic surgeons
· Vascular surgeons
· Anaesthetists
· Radiologists
· Cardiology
· Rheumatology
· Endocrinology
· Genetics
· Specialist nurses
· Psychologists
Professor Czerny went on to say:
“These new guidelines [also] describe the procedure for diagnosing and treating diseases of the aorta such as aortic aneurysm. If the aorta dissects, emergency surgery is required. "These diseases require complex surgical interventions, which we can better understand, research and perform thanks to the holistic view of the aorta," says Czerny. "Very good follow-up care is also very important, as those affected often show dangerous changes in the aorta again later in life,".
We have sought views from our Advisory Panel on this exciting development in the journey of the aorta.

Professor John Pepper opines:
“The aorta is a complex organ and not just a simple tube to enable the passage of blood from the heart to the rest of the aorta. The first part of the aorta is also a shock absorber which serves to reduce the power of the pulse so that by the time the blood reaches our organs; brain, gut, kidneys etc. the flow is almost continuous.
The wall of the aorta is made up of elastic tissue, muscle and a specialised type of jelly called the ExtraCellular Matrix or ECM for short. There is a lot of research going on into the ECM as it seems likely that small changes in this material in the Marfan aorta leads to enlargement of the aorta and eventually to the break-up of the elastic fibres. If these early changes can be detected by a simple blood test we would be able to anticipate such disasters as dissection or rupture, weeks or months before the event, and this would be much simpler and cheaper than performing frequent CT or MR scans. This lies in the future, but the future is not far away.”